Recently, an article in the Journal of Otolaryngology, Head and Neck Surgery, extrapolated data from a County hospital in Minnesota and calculated a national cost of inpatient hospital care for odontogenic deep neck space infections to be $200 million annually (1). Absent from this article was any mention of the cost or incidence of odontogenic rhinosinusitis. The reported incidence in the literature of dental pathology as a cause of rhinosinusitis is 10-12% (2). The primary source data for this incidence is from the 1950s and there is no documentation in the referenced articles of the data used to calculate this incidence. Therefore, the true incidence odontogenic rhinosinusitis is unknown and, based on my experience, most likely underappreciated.
Prior to reviewing odontogenic rhinosinusitis, we need to discuss common definitions. Rhinosinusitis is inflammation of the paranasal sinus and/or nasal cavities. This inflammation may be caused by allergic, infectious or immunogenic etiologies. Acute rhinosinusitis lasts up to 4 weeks, subacute rhinosinusitis lasts up to 12 weeks, and chronic rhinosinusitis lasts greater than 12 weeks. Acute rhinosinusitis is a clinical diagnosis based on the history and physical exam. Symptoms of sinusitis have been divided among major and minor factors (3). The diagnosis requires either two major factors or one major factor and 2 minor factors. Major factors include facial pain, facial congestion, nasal obstruction (blockage), purulent (discolored) nasal drainage (anterior or posterior), lack of or absence of smell, or fever. Minor symptoms include headache, fatigue, halitosis (bad breath), and dental pain, cough or ear pressure or pain.
| Major Symptoms | Minor Symptoms |
| Facial Pain | Headache |
| Facial Congestion | Fatigue |
| Nasal Obstruction | Halitosis |
| Purlent Drainage | Dental Pain |
| Loss of Smell | Cough |
| Fever | Ear Pressure/Pain |
Odontogenic rhinosinusitis is defined as sinusitis induced by a dental lesion. The common etiologies include periapical and periodontal disease, odontogenic lesions and iatrogenic and traumatic causes. Iatrogenic causes include complications of tooth extractions, implants, sinus augmentation, osteotomies and other orthodontic surgery, and a foreign body reaction to either the root canal sealant or filling material used in root canal therapy. A significant amount of literature is dedicated to complications associated with dental implants and sinus lifts. The reported incidence of rhinosinusitis resulting from sinus augmentation is 0-27% (4). However, when strict criteria are used to define rhinosinusitis, the incidence is 4.5%. Approximately 1/3 of these patients will progress from acute to chronic rhinosinusitis. Chronic rhinosinusitis requiring surgical intervention from sinus augmentation is reported to be 1.3% of patients(4). Sinus inflammation consisting of mucous membrane thickening on preaugmentation CT imaging is a statistically significant risk factor for post procedure acute or chronic rhinosinusitis (5). These are patients who would benefit from a preaugmentation ENT evaluation.
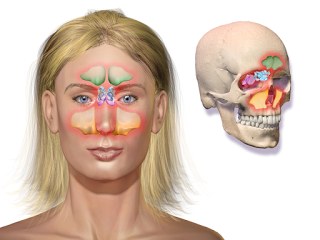
Prior to reviewing odontogenic rhinosinusitis, we need to discuss common definitions. Rhinosinusitis is inflammation of the paranasal sinus and/or nasal cavities. This inflammation may be caused by allergic, infectious or immunogenic etiologies. Acute rhinosinusitis lasts up to 4 weeks, subacute rhinosinusitis lasts up to 12 weeks, and chronic rhinosinusitis lasts greater than 12 weeks. Acute rhinosinusitis is a clinical diagnosis based on the history and physical exam. Symptoms of sinusitis have been divided among major and minor factors (3). The diagnosis requires either two major factors or one major factor and 2 minor factors. Major factors include facial pain, facial congestion, nasal obstruction (blockage), purulent (discolored) nasal drainage (anterior or posterior), lack of or absence of smell, or fever. Minor symptoms include headache, fatigue, halitosis (bad breath), and dental pain, cough or ear pressure or pain.
| Major Symptoms | Minor Symptoms |
| Facial Pain | Headache
|
| Facial Congestion | Fatigue |
| Nasal Obstruction | Halitosis |
| Purlent Drainage | Dental Pain |
| Loss of Smell | Cough |
| Fever | Ear Pressure/Pain |
Odontogenic rhinosinusitis is defined as sinusitis induced by a dental lesion. The common etiologies include periapical and periodontal disease, odontogenic lesions and iatrogenic and traumatic causes. Iatrogenic causes include complications of tooth extractions, implants, sinus augmentation, osteotomies and other orthodontic surgery, and a foreign body reaction to either the root canal sealant or filling material used in root canal therapy. A significant amount of literature is dedicated to complications associated with dental implants and sinus lifts. The reported incidence of rhinosinusitis resulting from sinus augmentation is 0-27% (4). However, when strict criteria are used to define rhinosinusitis, the incidence is 4.5%. Approximately 1/3 of these patients will progress from acute to chronic rhinosinusitis. Chronic rhinosinusitis requiring surgical intervention from sinus augmentation is reported to be 1.3% of patients(4). Sinus inflammation consisting of mucous membrane thickening on preaugmentation CT imaging is a statistically significant risk factor for post procedure acute or chronic rhinosinusitis (5). These are patients who would benefit from a preaugmentation ENT evaluation.
Treatment of sinusitis consists of saline irrigations, topical and systemic decongestants, antibiotics, topical and systemic steroids and allergy treatment. Antibiotics are used to treat acute rhinosinusitis and acute exacerbations of chronic rhinosinusitis. The specific antibiotic used is based on common microbiology patterns or the result of endoscopically-guided cultures. Recommended first-line antibiotics include Augmentin, high-dose amoxicillin, and extended spectrum cephalosporins. Surgery for acute or chronic rhinosinusitis is usually a last resort after maximal medical therapy has failed.

Odontogenic rhinosinusitis presents a unique challenge to the otolaryngologist. The diagnosis is frequently delayed. A dental source for the sinus infection is frequently not considered until after both medical and surgical therapy has failed to resolve the patient’s symptoms and radiographic disease. A primary cause for the delay in diagnosis is the failure of the radiologist and ENT physician to adequately assess dental pathology on CT imaging. In a 2010 retrospective case series involving 21 patients with known odontogenic rhinosinusitis, the initial radiology report failed to mention radiographic findings of dental pathology in 14 or 67% percent of the patients (6). There are symptoms which suggest an odontogenic source for the infection in patient presenting with rhinosinusitis. First, the large majority of patients will present with unilateral symptoms. This means that the patient will complain of nasal discharge, cheek pain, dental pain or nasal obstruction primarily on one side. Another unique symptom to odontogenic rhinosinusitis is a foul smell noted by the patient. In 76 patients with known odontogenic rhinosinusitis, 33 or 43% reported a foul smell (6,7,8).
In addition to early diagnosis, a successful outcome of odontogenic rhinosinusitis requires appropriate antibiotic therapy based on the common microbiology findings of a mixed polymicrobial infection. Like other odontogenic-induced infections, first-line antibiotic coverage for ORS is clindamycin. Additionally, successful treatment depends on eliminating the source of the infection. This requires early involvement of the dental health professional. In general, dental procedures take precedence over the ENT procedures. Situations where ENT surgery would precede dental surgery include the following:
- A complications of rhinosinusitis requiring emergent surgery.
- Sinus surgery in an infected maxillary sinus performed prior to closure of an oral antral fistula to increase the chance of success.
- Sinus surgery for pre-existing sinus disease prior to sinus augmentation (9).
The most important aspect of successful treatment consists of good coordination of care and communication between the dentist and ENT physician.
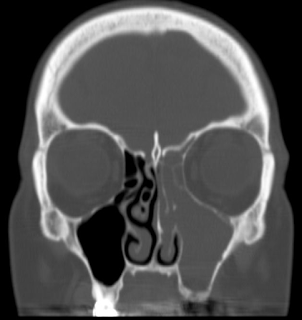
A 51 year old female presents with one year of left facial & tooth pain, left nasal obstruction, postnasal drainage and headaches. Past dental history is significant for RCT of teeth 10 & 11, apicoectomy of tooth #10, and dental implants #12 & 13. The implants failed and she developed an oral antral fistula after removal of the implants and debridement of necrotic bone. Coronal CT image demonstrating severe left maxillary and ethmoid sinus disease. This one sided sinus disease was of odontogenic origin.

